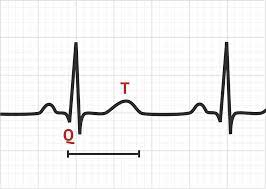
Medication interactions are a crucial aspect of healthcare that often demand vigilant attention. Among the myriad of potential complications, one of the most concerning is QT prolongation. QT prolongation refers to an abnormality in the heart's electrical cycle, specifically in the time it takes for the heart to recharge between beats. When this interval, known as the QT interval, is extended beyond normal limits, it can lead to a potentially life-threatening arrhythmia known as torsades de pointes.
This cardiac anomaly has garnered increasing attention in recent years due to its association with certain medications. While many drugs play essential roles in managing various medical conditions, some can inadvertently prolong the QT interval, predisposing individuals to cardiac arrhythmias. Understanding these medication interactions is paramount for healthcare professionals and patients alike to mitigate risks and ensure patient safety.
The QT Interval: A Brief Overview
Before delving into medication interactions, it's essential to grasp the significance of the QT interval. The QT interval represents the time it takes for the heart's ventricles to depolarize and repolarize, essentially the time from the start of ventricular contraction to the end of relaxation. It is measured on an electrocardiogram (ECG) and varies depending on factors such as heart rate, age, and gender. Typically, a QT interval of less than 450 milliseconds in men and 460 milliseconds in women is considered normal. Prolongation of this interval can disrupt the heart's rhythm, leading to potentially fatal arrhythmias.
Medications and QT Prolongation
Several classes of medications have been implicated in prolonging the QT interval, either independently or through drug interactions. Some of the notable drug classes include:
-
Antibiotics: Certain antibiotics, particularly macrolides (e.g., erythromycin, clarithromycin) and fluoroquinolones (e.g., ciprofloxacin, levofloxacin), have been associated with QT prolongation.
-
Antidepressants: Tricyclic antidepressants (e.g., amitriptyline, imipramine) and selective serotonin reuptake inhibitors (SSRIs) like citalopram and escitalopram can prolong the QT interval, especially at higher doses.
-
Antipsychotics: Several antipsychotic medications, including haloperidol, quetiapine, and risperidone, have been linked to QT prolongation.
-
Antiarrhythmics: Ironically, some drugs used to treat arrhythmias, such as certain class IA and III antiarrhythmics, can themselves prolong the QT interval.
-
Antiemetics: Ondansetron, commonly used to prevent nausea and vomiting, has been associated with QT prolongation, particularly in higher doses or when administered intravenously.
Risk Factors and Monitoring
It's important to recognize that not all individuals taking these medications will experience QT prolongation or related arrhythmias. However, certain risk factors may predispose individuals to adverse effects, including:
- Genetic predisposition: Some individuals may have genetic variations that make them more susceptible to drug-induced QT prolongation.
- Existing heart conditions: Patients with pre-existing heart conditions, electrolyte imbalances, or bradycardia (slow heart rate) may be at higher risk.
- Polypharmacy: Concurrent use of multiple medications that prolong the QT interval can increase the risk of adverse effects.
Regular monitoring of the QT interval via ECG may be warranted in high-risk patients or those taking multiple QT-prolonging medications. Additionally, maintaining electrolyte balance, particularly potassium and magnesium levels, is crucial in minimizing the risk of QT prolongation.
Clinical Implications and Patient Safety
Awareness of QT prolongation and medication interactions is paramount in clinical practice to ensure patient safety. Healthcare professionals should carefully evaluate patients' medication regimens, considering potential interactions and assessing individual risk factors. Shared decision-making with patients is essential, allowing them to understand the risks and benefits of prescribed medications.
Furthermore, healthcare providers should remain vigilant for signs and symptoms of QT prolongation, such as palpitations, dizziness, syncope (fainting), or sudden cardiac arrest. Prompt recognition and management of these symptoms can prevent adverse outcomes.
Conclusion
QT prolongation and medication interactions represent a complex and potentially life-threatening issue in clinical practice. While many medications are essential for managing various medical conditions, their potential to prolong the QT interval underscores the importance of careful prescribing, monitoring, and patient education. By fostering awareness and implementing appropriate risk mitigation strategies, healthcare professionals can minimize the incidence of drug-induced QT prolongation and ensure the safety and well-being of their patients.